Infectious Disease Data Science
I am an infectious disease physician and a data scientist. Assimilating diverse streams of data is critical to the practice of medicine, and I am passionate about leveraging technology to generalize the patient-doctor relationship to offer systems insights.My data science toolkit includes Python, pandas, NumPy, Matplotlib and scikit-learn. I previously studied at an immersive data science bootcamp through Galvanize inc., and earned a Masters of Science in Global Health at Duke University.Below you will find examples of data-driven projects I have produced in the domains of public health, patient education, and clinical research.
Antibiotic Utilization
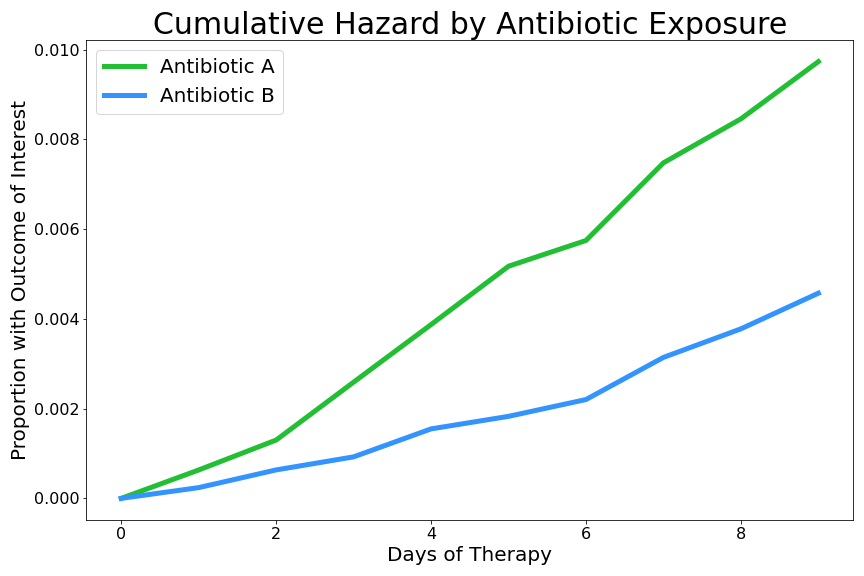
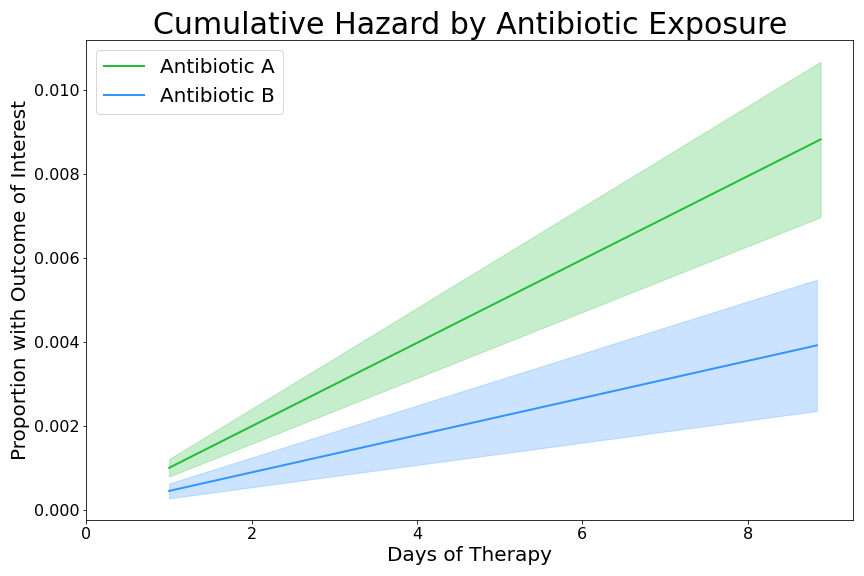
Broad-spectrum antibiotic exposure is a traditional risk factor for candidemia among hospitalized adults. Here, antibiotic spectrum indexing and time-to-event analysis are used to capture depth and breadth of antibiotic exposure. Cumulative hazard functions are plotted for a range of antibiotic agents and classes, and results are compared using Cox proportional hazard regression.Outputs are relevant to antibiotic stewards as well as mycology pathogenesis researchers. Below is a sample of the type of analysis I presented at Infectious Disease Week 2022. A video recording is available through the Infectious Disease Society of America.
Foodborne Disease Outbreaks
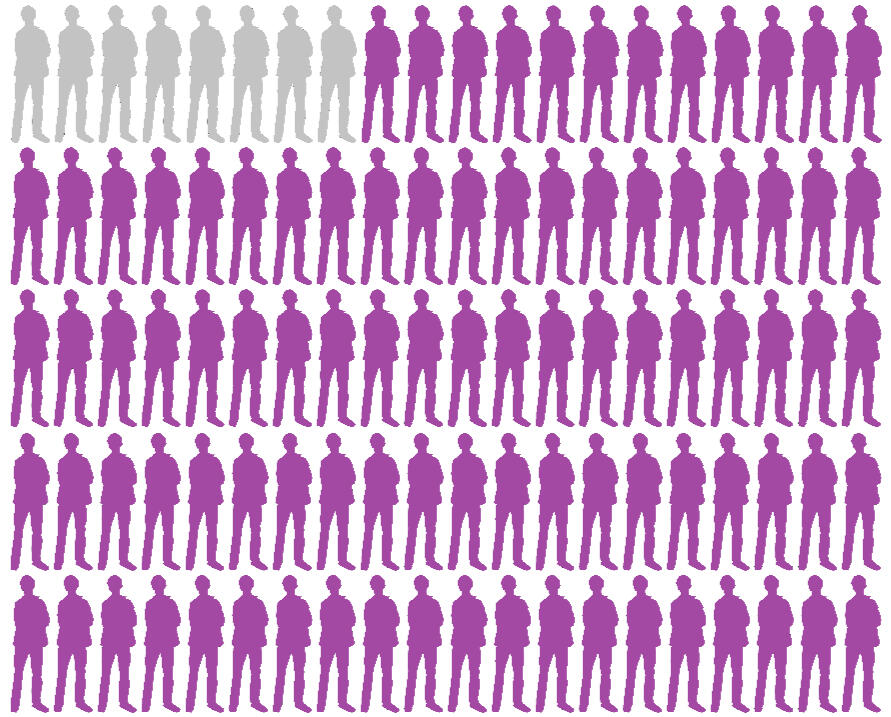
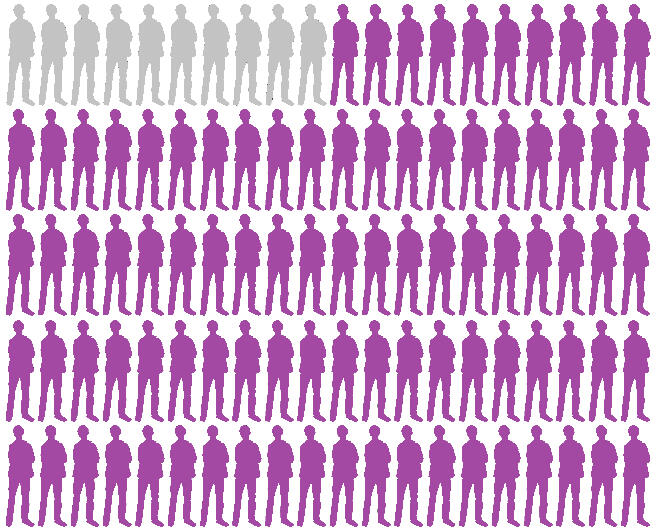
The CDC directs foodborne illness investigations, including detecting outbreaks, defining their size and extent, and identifying the source. These investigations are vital to both outbreak control and prevention. They collect data to characterize what ingredient is contaminated, where the food was prepared, which infectious agent is the culprit, and who had poor clinical outcomes as a result of exposure. Reportable disease data from 1998-2015 was used to create these visualizations for exploratory data analysis.
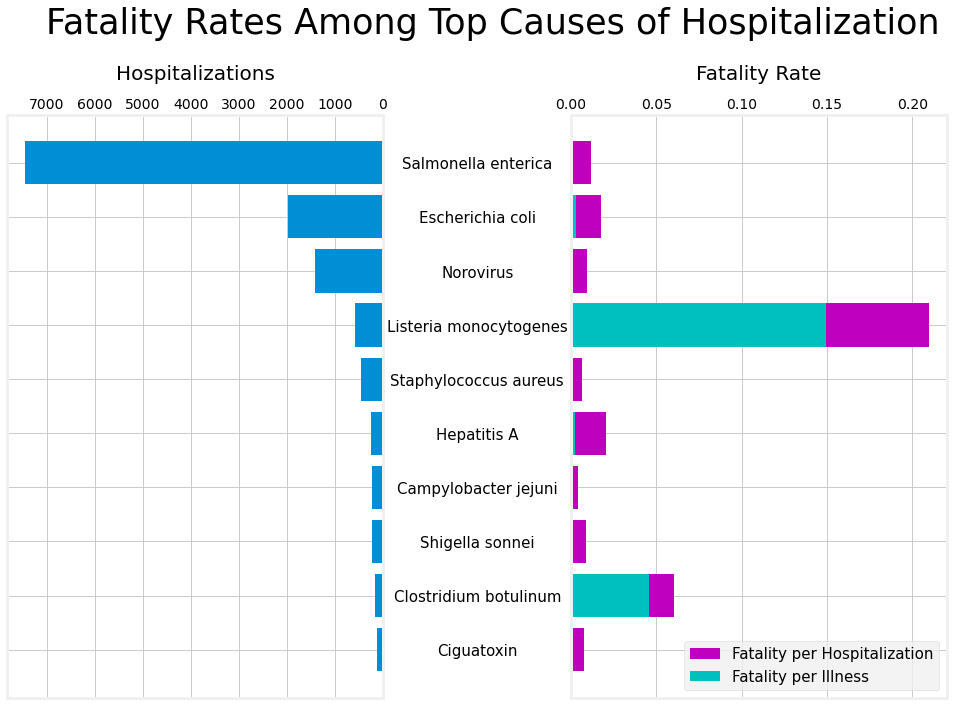

Data source: kaggle.com/datasets/cdc/foodborne-diseases
Decision Aids
Vaccine misinformation is a major challenge to people accessing preventive healthcare services. These leaflets are meant to be displayed in primary care clinics, where they can serve as conversation starters with vaccine-hesitant patients by highlighting the potential benefits of vaccines while also acknowledging their limitations. Their design incorporates best practices for data visualization that is accessible to a wide audience.
Vaccine Acceptance
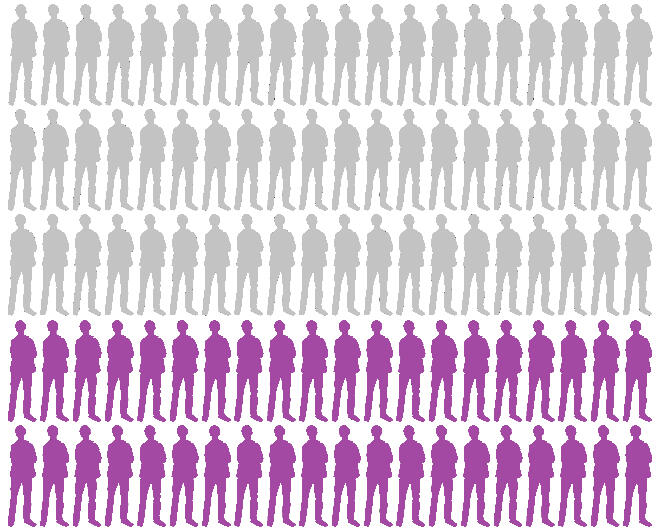
Should I get vaccinated?
Volume 3: Tdap
(Tetanus, Diphtheria, Pertussis)
What is pertussis?
Pertussis, also known as whooping cough, causes severe coughing spells, which can cause difficulty breathing, vomiting, and disturbed sleep. It can also lead to weight loss, incontinence, and rib fractures. Some adults are hospitalized or have complications, which could include pneumonia or death.
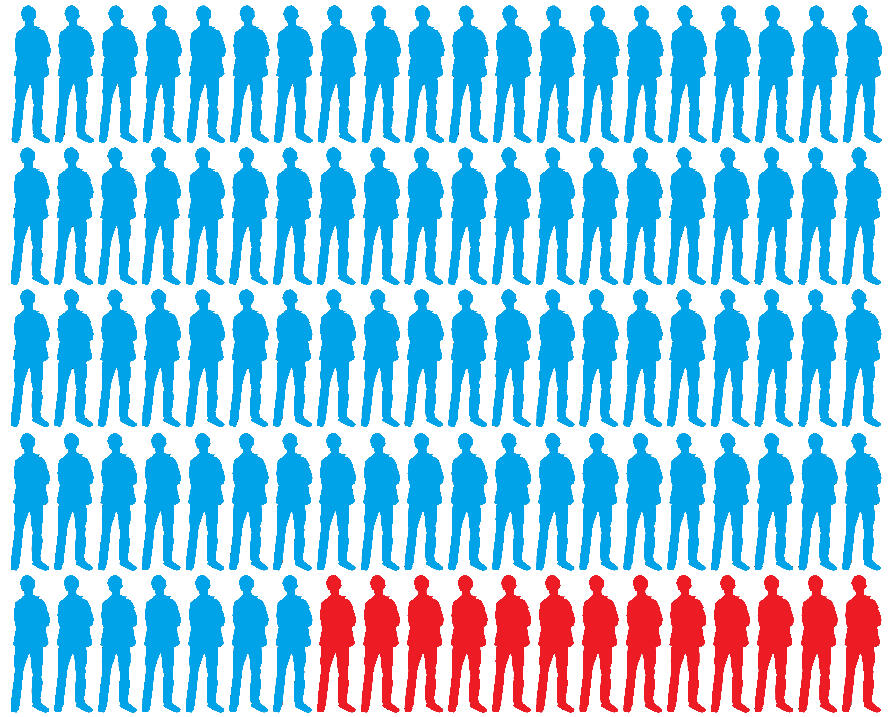
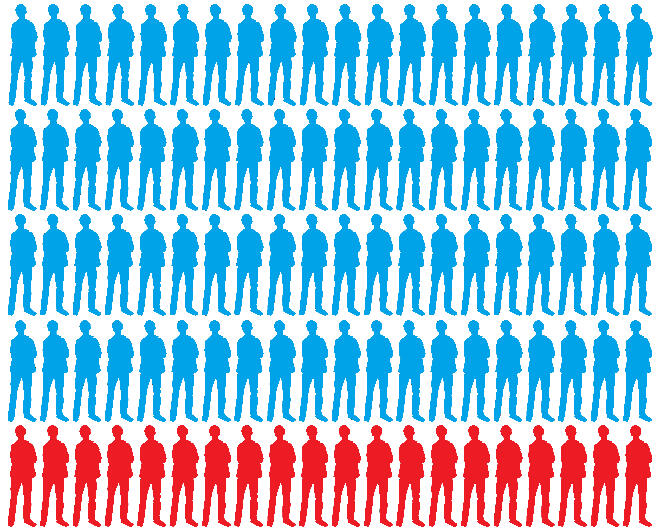
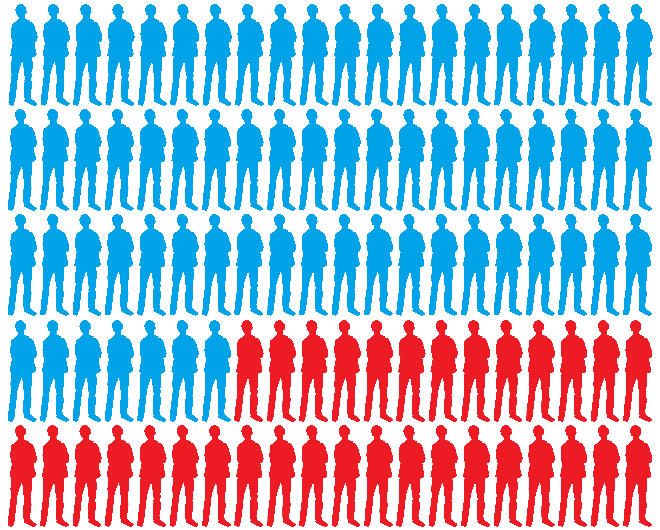
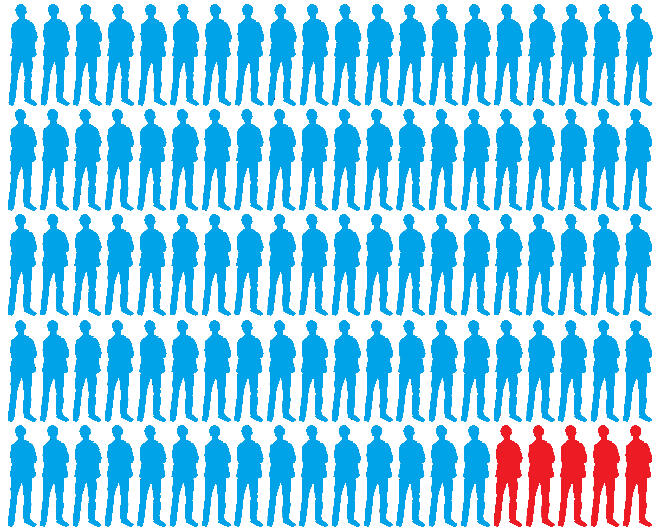
92 out of 100 patients who are vaccinated against pertussis are protected from the infection.
What is tetanus?
Tetanus, also known as lockjaw, causes painful muscle tightening and stiffness. It can lead to tightening of muscles in the head and neck so you can’t open your mouth, swallow, or sometimes even breathe.
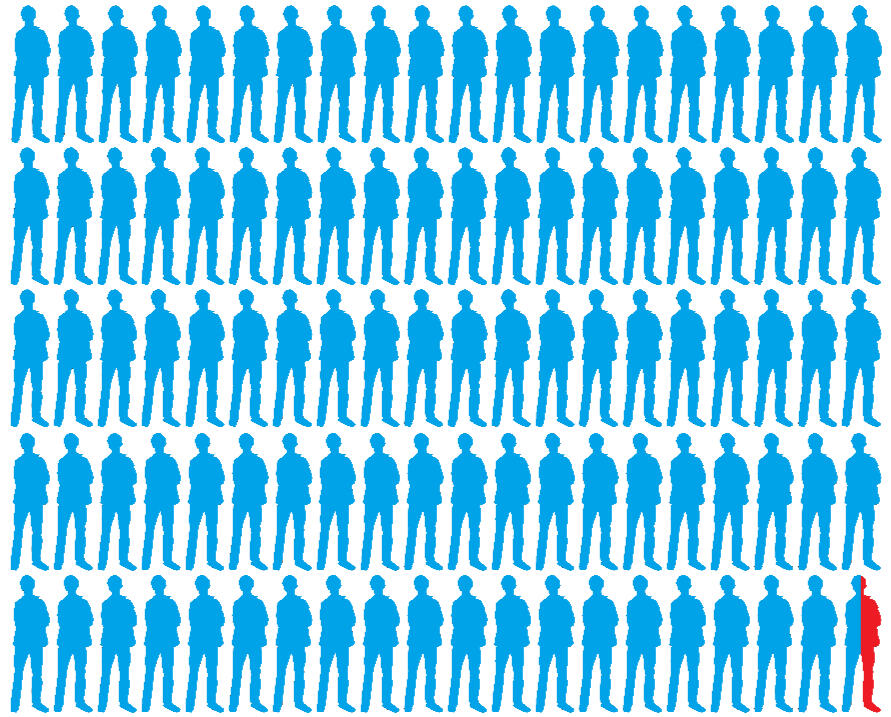
If you are exposed to tetanus but have not been vaccinated, then you have a 13% chance of dying from the infection.
If you are exposed to tetanus and you are vaccinated, then you have a less than 1% chance of dying from the infection.
What is diphtheria?
Diphtheria is a bacteria that causes a thick coating to form in the back of the throat. It can lead to breathing problems, heart failure, paralysis, and death. Diphtheria was once a greatly feared illness in the United States. In the 1920s, there were between 100,000 and 200,000 cases each year. Because of widespread immunization and better living conditions, diphtheria is now rare in the United States.
Some people should not get vaccinated
Life threatening allergic reaction to a previous dose
Coma or seizures within seven days of a previous dose
Guillain-Barré syndrome within 6 weeks after a previous dose
Data source: cdc.gov/vaccines/hcp/vis/
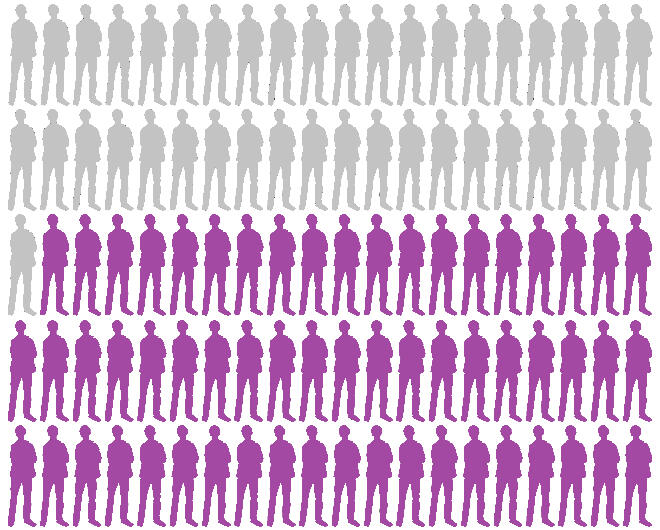
Should I get vaccinated?
Volume 2: Shingles
What is shingles?
Shingles is a painful rash that usually develops on one side of the body, often the face or torso. The rash consists of blisters that typically scab over in about a week and clear up in about a month. For some people, the pain can last for months or even years after the rash goes away.
How well does the vaccine work?
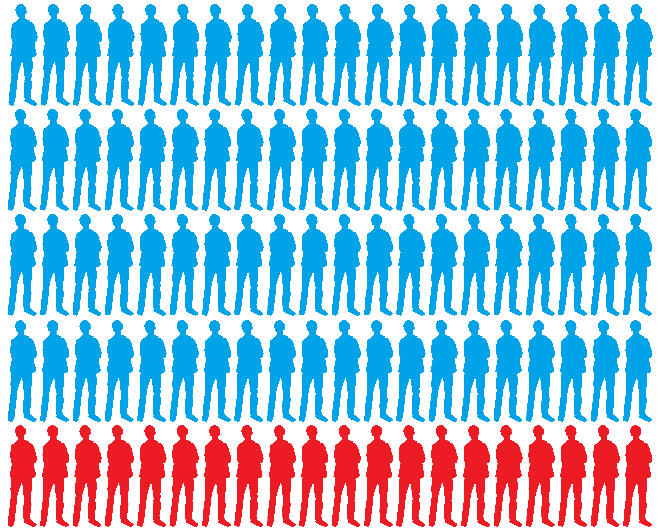
90 out of 100 patients who are vaccinated against shingles are protected from the disease.
How common is it?
1 in 5 people experience severe pain even long after the rash has cleared.
Over 1 million people in the United States get shingles every year. 1 out of every 3 people will develop shingles in their lifetime.
Some people should not get vaccinated
Life threatening allergic reaction to a previous dose
Tested negative for immunity to varicella zoster virus
Currently have shingles
Pregnant or breastfeeding
Receiving more than low-dose immunosuppressive therapy
What are the side effects?
Most people have a sore arm with mild or moderate swelling
Some people feel tired, have muscle pain, headache, fever, chills, stomach pain, or nausea
Side effects are more common in younger people
Severe side effects are extremely rare (1-2 per million doses)
Data source: cdc.gov/vaccines/hcp/vis/
Should I get vaccinated?
Volume 1: Pneumococcus
What is pneumococcus?
Pneumococcal pneumonia (lung infection) is the most common disease caused by pneumococcus bacteria. Symptoms include abrupt onset of fever, shaking chills or rigors, chest pain, cough, shortness of breath, rapid breathing and heart rate, and weakness.It can also cause infection of the bloodstream (bacteremia) and infection of the lining of the brain and spinal cord (meningitis).
How common is it?
Every year in the United States, 18,000 older adults die of pneumococcal disease, and pneumococcal pneumonia alone accounts for 400,000 hospitalizations.
How is spread?
The bacteria can spread from person to person by direct contact with respiratory secretions, like saliva or mucus. People can carry the bacteria in their nose and throat, and can spread the bacteria without feeling sick.
How deadly is pneumococcus?
Pneumococcal pneumonia kills about 1 in 20 people who get it.
Pneumococcal meningitis and bacteremia kill about 1 in 5 people who get either.
How well do the vaccines work?
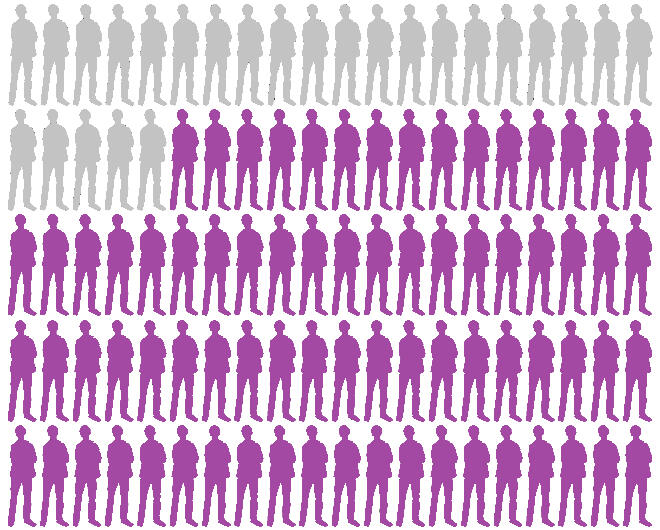
45 in 100 patients who are vaccinated are protected from pneumonia.

75 in 100 patients who are vaccinated are protected from meningitis and bacteremia.
Some people should not get vaccinated
Life-threatening allergy to prior dose of pneumococcal or diphtheria toxoid vaccines
Pregnant women
What are the
side effects?
Some adults have pain, redness and swelling of the arm
Less than 1 out of 100 adults develop fever, muscle aches, or more severe local reactions
Who should be vaccinated?
Everyone 65 and older should be vaccinated against pneumococcus. Younger adults should be vaccinated if they have any of the following:
Weakened immune system
Asthma
Heart disease
Diabetes
Kidney failure
Sickle cell anemia
Lymphoma
HIV/AIDS
Asplenia
Alcoholism
Cigarette smokers
Data source: cdc.gov/vaccines/hcp/vis/
Should I get vaccinated?
Volume 4: Flu
What symptoms does influenza cause?
Fever
Muscle aches
Stuffy/runny nose
Cough
Headache
Fatigue
Sore throat
What are common side effects of the
flu shot?
Fever
Sore arm
Red/itchy eyes
Cough
Headache
Fatigue
Hoarse voice
Do you notice a pattern?
So, why consider a flu shot?
Vaccination prevents 40 out of 100 people who get the flu from needing to be hospitalized.
Vaccination prevents 59 out of 100 hospitalized flu patients from needing the intensive care unit.
Some people should
not be vaccinated
Ongoing moderate to severe illness
History of Guillain-Barré Syndrome after receiving a prior flu vaccine
Can you get influenza
from the flu shot?
No, the vaccine contains inactivated viral particles
The vaccine can cause side effects that mimic flu-like symptoms but does not cause dangerous infection
I have an egg allergy.
Can I get the flu shot?
Yes, modern flu shots are well tolerated by people with mild to moderate egg allergy
Even patients with severe egg allergy can get the flu shot, in a monitored setting
When should you
be vaccinated?
Every year
Two weeks before the start of flu season (October), but better late than never
Data source: cdc.gov/vaccines/hcp/vis/






